Clin Exp Rheumatol Review Neuro Behcets Disease Its Mimickers and
In March 2017, a mini-symposium at the 11th Congress of Controversies in Neurology (CONy), Athens, Greece, was defended to neuro-Behçet's affliction (NBD). An introduction into the central clinical features of Behçet'south disease (BD) was followed by a review of its neurological manifestations and a focused presentation of the challenges of differential diagnosis. This review represents a report of the mini-symposium in the form of an updated summary of the topics that were presented. It follows the construction of the mini-symposium and in part expands the information presented there. Withal, a systematic review is beyond the scope of this report. The full general introduction to BD volition exist succinct, as the focus of this review is NBD. Details of BD in general can exist plant in recent reviews, for instance, Yazici et al.i
Behçet's disease
History and epidemiology
BD is a chronic, multisystemic and polysymptomatic disease with unpredictable exacerbations and remissions. All systems tin can be afflicted concomitantly or consecutively.1 There are several clinical subsets and there is geographical variation indicating different affliction mechanisms. In view of this, some authors favour using the term Behçet'southward syndrome rather than Behçet's disease. For consistency and harmonisation purposes, and to follow the terminology of the discussions of the mini-symposium, this review will use the term Behçet's disease. In 1930, the ophthalmologist Adamantiades described the coexistence of ocular, skin and mucous lesions in one patient.ii In 1937, Hulusi Behçet identified BD in two patients, who were suffering from oral and genital ulcers, in addition to eye affliction and described it as a separate illness believed to be caused past a virus.three
Epidemiologic studies accept shown a broad variability in the prevalence of BD depending on the geographic and ethnic origins of the population. Prove shows that the prevalence of BD is college in the areas in which the population has a high incidence of HLA-B51 allele.four It is oft chosen 'silk route affliction' because of its relatively high prevalence in Mediterranean, Center Eastern and Far Eastern countries across the aboriginal silk trading road. Turkey has the highest prevalence, at 119.8 per 100,000.4
Pathophysiology
The pathomechanisms of BD are not fully known; however, it can be viewed equally a condition associated with autoimmune responses, autoinflammation and vascular injury. Susceptibility seems to be adamant by an interplay betwixt genetic and environmental factors. Among the susceptibility genes, those for cytokines such as interleukin (IL)-17, IL-12, IL-23, IL-21, IL-23, tumour necrosis factor (TNF)-α, IL-1β and IL-viii have been implicated.five Dysregulation of these pro-inflammatory cytokines may reflect an uncontrolled activation of the innate immune system with or without activation of the adaptive allowed responses that appear to be responsible for the pathological features. Elevated production of pro-inflammatory cytokines, such as TNF-α, IL-1β and IL-eight, results in the activation of neutrophils and the augmentation of cellular interactions between neutrophils and endothelial cells.half-dozen These activated neutrophils produce excessive superoxides and lysosomal enzymes which bring about tissue injury. The resulting lesions are characterised histologically by neutrophilic angiocentric infiltrates with leukocytoclastic (early) or lymphocytic (belatedly) vasculitis with or without mural thrombosis and necrosis.7 In improver, B lymphocyte function has been reported to be abnormal in some patients.8
Among the environmental factors responsible for susceptibility to BD, infectious agents that have been implicated almost ofttimes include bacteria such every bit Streptococcus sanguinisand viruses, mainly herpesviruses. Indeed, the gene–environment interaction in BD is indicated by dumbo genotyping studies linking dysregulated host allowed response to bacterial antigens to the BD susceptibility.9
Clinical manifestations and diagnosis
BD has a wide range of clinical manifestations. Oral ulcers are normally the starting time symptom; they may announced years before the diagnosis and are present during the disease class at almost 100% frequency. In 75% of patients, anogenital aphthae are seen, primarily on the scrotum and penis in men and the vulva in women. In effectually 60% of patients, various cutaneous lesions have been reported, which include erythema nodosum, papullopustular lesions, pseudofolliculitis, pyoderma gangrenosum, and cutaneous vasculitis.1,10
In improver, numerous other areas are commonly affected by BD. Ocular presentations of BD occur in 30–fourscore% of patients (predominantly in men) and are a major cause of morbidity as they can result in blindness, peculiarly in the setting of retinal vasculitis.ane Articulation involvement is too ordinarily reported in BD. Mono/polyarthritis in BD is Italicsnon-erosive and the most afflicted joints are knees, ankles, feet and Italicshands. Gastrointestinal involvement is characterised by pain, bleeding, gut mucosal ulcerations or abdominal perforation. ItalicsVascular involvement may also occur, virtually commonly deep/superficial peripheral venous thrombosis and too aneurysmal/occlusive arterial disease. Cardiac interest includes coronary arteritis, vascular disease, intracardiac thrombi or thrombosis of venous collateral vessels and superior vena cava, myocarditis and recurrent ventricular arrhythmias.1 Neurological involvement is also a common manifestation of BD, and will be discussed farther in the following section.
The diagnostic criteria for BD were published 28 years ago.11 The major criterion is recurring oral ulcerations (aphthous or herpetiform) observed by the physician or reliably reported by the patient at to the lowest degree three times in a 12-month menses. In addition, ii of the 4 minor criteria must exist fulfilled:
- recurrent genital ulceration;
- center lesions: inductive uveitis, posterior uveitis, cells in the vitreous by slit lamp examination or retinal vasculitis observed by an ophthalmologist;
- pare lesions: erythema nodosum, pseudofolliculitis, papulopustular lesions or acneiform nodules in post-adolescent patients not on corticosteroids; and
- a positive pathergy test (skin prick exam): not-specific peel Italicshyper-reactivity in response to minor trauma read past a physician at 24–48 hours (>2 mm pustule, after forearm skin (v mm depth) prick with twenty–22 g needle).
Treatment options
The goal of BD handling is to promptly suppress inflammatory exacerbations and recurrences to prevent irreversible organ harm and a multidisciplinary approach is necessary. The direction of BD depends on whether there are self-limiting manifestations or serious organ interest, and should be individualised according to age, gender and blazon.12,thirteen In systemic severe disease, intravenous pulse corticosteroids followed past daily oral doses, azathioprine, cyclophosphamide, cyclosporine-A, methotrexate, mycophenolate mofetil, tacrolimus, interferon (IFN)-α or TNF-α inhibitors (etanercept, infliximab) can be chosen.12 A new oral inhibitor of phosphodiesterase-four, apremilast, has been studied in patients without major organ involvement and demonstrated a complete response in significantly more than patients.14
Other treatments aim to control the specific symptoms of BD. TNF-α inhibitors are highly effective in BD, particularly in ocular involvement.fifteen,16,17 Long-term assistants of the TNF-α inhibitor infliximab may reduce the frequency of ocular recurrences, even in resistant cases. Every bit a first-line treatment, infliximab should be started in conjunction with an immunosuppressive drug (azathioprine, corticosteroids or Italicsmethotrexate) and upon occurrence of remission, concomitant corticosteroids should be reduced. Many studies have demonstrated the effectiveness of infliximab in BD.15–17 In patients with posterior segment heart involvement, azathioprine, cyclosporine-A, IFN-α or anti-TNF-α oft combined with systemic corticosteroids, should be initiated. In patients with posterior segment eye involvement, azathioprine, cyclosporine-A, IFN-α or anti-TNF-α frequently combined with systemic corticosteroids, should exist initiated.12,13
For the direction of major vessel affliction with thrombotic events in BD, corticosteroids and immunosuppressants such every bit azathioprine, cyclophosphamide or cyclosporine-A are recommended,12 and Italicsanti-TNF-α could be considered in refractory patients. Anticoagulants are considered when the adventure of haemorrhage, in general, is low and coexistent pulmonary artery aneurysms are ruled out.12,13 For gastrointestinal symptoms, 5-aminosalicylic acid derivatives, including sulfasalazine or mesalamine, systemic corticosteroids, azathioprine, anti-TNF-α, and thalidomide may exist used. Fundamental nervous arrangement interest, including astute attacks of cerebral parenchymal involvement, are treated with loftier-dose corticosteroids followed by tapering, together with immunosuppressants. Cyclosporine, although inexpensive, should be avoided due to the risk of neurotoxicity. Anti-TNF-α should be considered in severe or refractory disease as Italicsfirst-line. The first episode of cerebral vein thrombosis (CVT) should be treated with loftier-dose corticosteroids, followed past tapering. Anticoagulants may exist added for a short elapsing.
Neurological involvement in Behçet's disease
As with systemic disease, the neurological manifestations of BD are varied.18–22 Neurological involvement in BD can exist classified as; 1) primary, in which the neurological involvement is directly due to BD and is named as NBD or neuro-Behçet's syndrome (NBS); and 2) secondary, in which the neurological manifestations are the effect of neurologic complications secondary to systemic interest of BD (i.east. cerebral emboli from cardiac complications of BD, increased intracranial pressure secondary to superior vena cava syndrome) or due to the therapies used for the systemic manifestations of BD (i.east. central nervous organisation [CNS] neurotoxicity with cyclosporine; peripheral neuropathy secondary to thalidomide or colchicine). These are indirect causes of neurological problems in patients with BD and are non termed as NBD.
Primary neurological involvement with NBD occurs in up to 10% of all patients.xviii–22 NBD unremarkably presents within the quaternary decade and approximately five years afterwards the onset of the systemic disease. Although some patients may present with neurological involvement without fulfilling the International Study Group (ISG) nomenclature criteria for BD,11 and a diagnosis of NBD cannot typically be made unless there are at least the history or sequelae of some of the systemic manifestations of BD. Although BD is seen almost equally in both genders, NBD is more common in males (iii:1).23 BD and NBD are rare in the paediatric population; however, when neurologic interest occurs in children it is often soon later on the onset of the systemic disease.twenty.21
Clinical and neuroimaging findings signal that at that place are 2 major forms of NBD: 1) CNS inflammatory parenchymal disease (p-NBD); and, less commonly, 2) an extra-parenchymal class (ep-NBD) that involves large extra-parenchymal vascular structures, mainly venous dural sinuses, causing cerebral venous sinus thrombosis (CVST). In contrast to p-NBD, CVST is more commonly observed in paediatric patients with NBD and these two types of involvement occur very rarely in the same private and, thus, are likely to have unlike pathogeneses. Rarely, an aseptic meningitis may exist the presentation of extra-parenchymal NBD. Behavioural and psychotic symptoms, which are termed as 'neuro-psycho-Behçet', may be observed during the form of NBD. Cognitive functions are besides probable to be affected in a subgroup of patients with BD and frontal (executive) dysfunction is the most common pattern observed. Principal peripheral nervous system involvement has been reported in BD, but is extremely rare.18,nineteen
The almost common neurological symptom seen in NBD is headache, which occurs both in parenchymal (p-NBD) and extra-parenchymal NBD (ep-NBD, CVST). However, headache may also be a symptom of astringent ocular inflammation; may be associated with exacerbations of systemic symptoms of BD, with some migraine-like features, and is referred to as the 'nonstructural headache of BD'; or may be independent of BD and may coexist every bit a primary headache at like rates with the general population. Other common symptoms are weakness (hemiparesis), gait disturbances (clutter), speech difficulties (dysarthria) and less commonly, behavioural and cognitive changes. Visual loss due to optic neuritis, sensory and extrapyramidal symptoms and seizures are rare.18–22
The International Consensus Recommendation (ICR) criteria are suggested to exist used in diagnosing NBD.24 These criteria tin can exist summarised as 'the occurrence of neurological symptoms and signs in a patient who meets the ISG Diagnostic Criteria for BD that are not otherwise explained by whatsoever other known systemic or neurological affliction or handling and in whom objective abnormalities consistent with NBD are detected either on neurological examination, neuroimaging studies, MRI, or abnormal cerebrospinal fluid (CSF) examinations'.24 The ICR criteria also include a 'probable NBD' criteria, but one should be more than prudent in making such a diagnosis.
Parenchymal neuro-Behçet'due south disease
Nigh 75–80% of patients with NBD present with parenchymal involvement. The major symptoms and signs of p-NBS include headache, dysarthria, ataxia, hemiparesis and cranial neuropathies (mainly involvement of motor-ocular and facial nerves) and these usually develop in a subacute manner. p-NBD is one of the major causes of morbidity and bloodshed in NBD. Similar to multiple sclerosis (MS), the clinical course of p-NBD may remain with a single attack, may have a relapsing grade, or may be progressive. However, patients with p-NBD unremarkably are left with neurologic deficits. The lesions of p-NBD lesions commonly involve the telencephalic/diencephalic junction and the brainstem, which are commonly large, with no singled-out borders. In the acute phase these lesions are likely to enhance and generally appear in a heterogeneous design. Tumefactive cognitive lesions may be seen, and spinal cord lesions, although not common, when occurring are likely to be longitudinally all-encompassing. In these patients, anti-MOG and AQP4 antibodies are typically absent-minded. Cerebellar focal interest is uncommon, but isolated cerebellar cloudburst has been reported.25 Lesions in intra-parenchymal major arterial territories are unusual and involvement of large extra-parenchymal or smaller intra-parenchymal arteries although extremely rare have been reported, suggesting that a subgroup of arterial p-NBD may exist.26 Based on the radiological and histopathological findings, a venous pathogenesis is the likely explanation of p-NBS lesions.17–19,26
The CSF findings may disclose a prominent pleocytosis and an elevated protein level during the acute episode of p-NBD. Neutrophilic predominance is typical during the astute phase, merely this after is replaced past a lymphocytic class. Oligoclonal bands are rarely detected.
Extra-parenchymal neuro-Behçet's disease/cognitive venous sinus thrombosis
Up to 20% of patients with NBD take CVST. These patients nowadays with severe headache, which usually develops over a few weeks. Typically, the funduscopic and neurological examination shows papilledema and occasionally a 6th nervus palsy. Compared with other causes of dural sinus thrombosis, dumb consciousness, focal neurologic deficits such as hemiparesis and epileptic seizures are uncommon in actress-parenchymal NBD, and venous infarcts are unlikely. A magnetic resonance venography will confirm the diagnosis and evidence the extent of CVST. With the exception of an elevated opening pressure, the CSF findings are generally normal, except in the rare meningitic presentation where a high number of neutrophils can be found. Equally already mentioned this class of NBD occurs more than commonly in the paediatric population suggesting that age may influence the class of neurological involvement.
Neuro-Behçet's disease – differential diagnosis
The differential diagnosis of NBD remains a major challenge. Especially hard are situations in which a patient without full blown BD presents with neurological manifestations. It is of import to know that neurological manifestations of BD reflect more severe affliction, and are rarely seen in isolation. Therefore, clinicians suspecting NBD must be vigilant to look for the likely evolution of symptoms and signs exterior the CNS. This is also important in patients with known BD, as neurological manifestations tend to announced during severe flare-ups, and systemic BD manifestations should be sought. In meningitic presentations, the differential diagnosis from acute bacterial meningitis is essential. Astute bacterial meningitis is a medical emergency and antibiotic treatment is often initiated in emergency settings before the microbiological confirmation. Although the CSF in meningitic NBD often has fewer leucocytes, information technology tin sometimes accomplish the numbers encountered in bacterial meningitis and failure of recognition may have serious consequences. A transient clinical improvement can exist seen following institution of supportive measures and antibiotics, which may delay the aggressive treatment of BD.
Uveomeningeal syndromes are a heterogeneous group of inflammatory disorders characterised by meningeal inflammation and middle involvement (uveitis).27 The differential diagnosis includes many entities, and associated systemic features, specific organ involvement (eastward.chiliad. lung in sarcoidosis) and imaging and biomarker characteristics tin can aid distinguish NBD from the other conditions. In add-on to NBD, uveomeningeal syndromes include:
- sarcoidosis;
- granulomatosis with polyangiitis;
- syphilis;
- Vogt-Koyanagi-Harada disease; and
- acute posterior multifocal placoid pigment epitheliopathy.
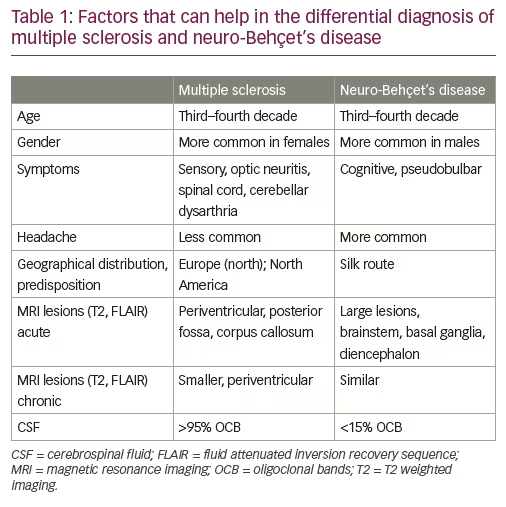
One of the almost important and challenging considerations in the differential diagnosis of NBD is MS.xviii,28 When the diagnosis for either entity is well established, distinction is relatively easy; notwithstanding, in the initial phases, the stardom can be hard. The parenchymal lesions of NBD can mimic those of MS on MRI in nigh aspects, including the ovoid shape of callosal 'Dawson'southward fingers' and the presence of a central vein. Due to the perivenular distribution of lesions in both conditions, the utility of the central sign and its part in the differential diagnosis of MS versus NBD remains subject to debate in expert consensus discussions.28,29 While this is particularly relevant early in the affliction and recent evidence shows that more MS than NBD white matter lesions have cardinal veins, one needs to bear in mind that mostly, patients with NBD accept fewer white matter lesions than patients with MS, so using the key vein for stardom may remain difficult. Other issues that take been helpful in distinguishing the two entities can exist seen in Table 1. It is important to note that the initial manifestation of NBD can be a tumefactive brain lesion, which can be most indistinguishable from both a tumefactive MS presentation and a brain neoplasm, the latter being an essential differential diagnosis consideration.30,31 Clinicians need to exist aware that NBD and MS need not exist mutually exclusive. Indeed, a group of patients with established NBD as well fulfil the diagnostic criteria for MS and have clinical, imaging and laboratory features (oligoclonal bands in the CSF) of MS.32
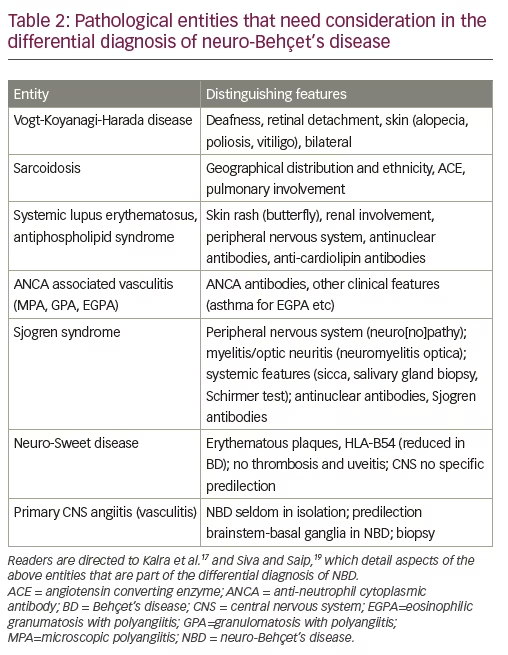
Another of import attribute of the differential diagnosis is systemic vasculitis, which can be chief or secondary to other systemic inflammatory diseases with neurological manifestations. Tabular array two presents a list of systemic inflammatory disease with or without secondary vasculitis which can be misdiagnosed as NBD and their distinguishing features which tin can help in the differential diagnostic of NBD. These are discussed in more detail in Kalra et al. and Siva and Saip.eighteen,24
In patients presenting with acute stroke, the vascular variant of NBD sometimes represents office of the differential diagnosis. To distinguish from non-vasculitis atherosclerotic stroke, it is helpful to bear in mind the higher frequency of venous thrombosis compared to arterial territory stroke in NBD. On the other mitt, some strokes in NBD involve arterial territories, then an arterial stroke can be a manifestation of NBD. Information technology is also important to remember that patients with BD are at college risk of cardiovascular events including stroke, independent of whether they have NBD.33 Arterial dissections and bleeds, admitting relatively rare in NBD, should trigger suspicion of information technology in the appropriate clinical setting.
Psychiatric NBD is a rare manifestation, ordinarily with a subacute, progressive presentation, and has highly diverse manifestations, mimicking primary degenerative dementia, depression or frank psychosis. It is very important to consider NBD in such patients.34
An of import aspect of the differential diagnosis is the evolution of a neurological problem in a patient with established BD. The clinicians need to establish whether or not the trouble is related to NBD. Too stroke, headache is a very mutual complaint in people with BD and it does not mostly stand for a manifestation of NBD. Vigilance is needed, still, as headache oft heralds other manifestations of NBD.
Peripheral neuropathy occurs rarely as a clinical manifestation of NBD and when diagnosed in a person with BD and no other neurological manifestations, a search for culling aetiologies is warranted.35
Finally, an emerging differential diagnosis aspect concerns neurological complications of BD treatment. It is critical not to mistake such complications for the development of NBD. The role of cyclosporine in NBD is of import as information technology has been linked consistently to a potential acceleration and worsening on NBD. Other treatments also may take complications. Immunosuppressive agents may occasionally facilitate meningitis, which can be confused for NBD. The use of anti-TNF agents such as infliximab, which has been shown to be successful in NBD,36 should crave vigilance, as demyelination and other neurological complications take been reported with these agents, although none nonetheless has been reported with use in BD.
Thalidomide, which is occasionally used for BD, predictably causes a neuropathy which is not related to NBD. Posterior reversible encephalopathy syndrome has been reported every bit a complication of several immune therapies including anti-TNF agents, and at the 2017 CONy symposium, an interesting instance in BD was reported past Dr George Vavougios from Greece (Oral advice, CONy Congress, Athens 2017).
In conclusion, NBD is a serious neuroinflammatory condition which poses major diagnostic, differential diagnostic, and therapeutic challenges. Awareness of its clinical features and therapeutic possibilities together with early diagnosis are essential in the management of NBD.
Source: https://touchneurology.com/neuromuscular-diseases/journal-articles/neuro-behcets-disease-clinical-features-diagnosis-and-differential-diagnosis/
0 Response to "Clin Exp Rheumatol Review Neuro Behcets Disease Its Mimickers and"
Post a Comment